As a Community Health Plan of Washington (CHPW) provider, you can count on our support in caring for your patients. Find answers to questions you may have about our provider portals, training and orientation materials, and more.
How can I become a Community Health Plan of Washington provider?
To join our network, please fill out and submit an online Provider Enrollment form. We will review your information and contact you within 30 days. If you have questions, please contact our Provider Relations department at [email protected].
Where can I find out more information on Provider Portals?
We want to make it easy for you to care for your patients. Use our Provider Portals page to submit and view requests, access patient information, and stay on top of your paperwork.
For portal-specific support, please contact [email protected].
How do I know if a drug I prescribe is on the formulary?
You can review the formulary on our Prescription Drug Coverage page to identify which drugs are covered by CHPW and which require preauthorization. Drugs not listed on our formulary require prior authorization. You can submit prior authorization requests through our Care Management Portal (Jiva).
For self-administered drugs requiring prior authorization, please call 1-800-753-2851.
How do I submit a Prior Authorization request?
Providers should submit prior authorization through Care Management Portal (Jiva).
You can also fax prior authorization requests to 206-652-7065. Please check the fax number located at the top of each form as it may differ depending on the request. Find CHPW Prior Authorization forms here.
For pharmacy, providers should submit requests via ExpressScripts for prior authorization, step therapy, non-formulary, or quantity limit override. Call them at 1-800-922-1557 to speak with a prior authorization specialist. For professionally administered drugs follow instructions here.
All other prior authorization requests will be handled by CHPW staff. Please contact your provider relations representative for more information.
Who do I contact for claim status, prior authorization, member benefits, or member eligibility?
Providers can get in touch with our Provider Relations department at [email protected] or contact Customer Service for assistance at 1-866-907-1906 (TTY Relay: 711) Monday through Friday from 8 a.m. to 5 p.m.
I have a patient who missed their appointment without warning. Can I still bill them?
No. Patients cannot be billed for missed appointments. Make sure they are aware of your clinic’s cancellation or late appointment courtesy policies.
My patient needs to see an out-of-network specialist. Can I still refer them?
Any request to see a non-network provider requires CHPW approval, regardless of whether the service requires prior authorization.
MemberFirst™ Rewards Program
What is the CHPW MemberFirst™ Rewards Program?
MemberFirst™ is CHPW’s new member incentives program created to encourage CHPW members to get preventive screenings.
Similar to the CHPW Apple Health (Medicaid) ChildrenFirst™ program, CHPW members can earn gift card rewards for completing recommended health services.
To claim rewards, eligible CHPW members fill out an online form after completing a qualified cancer screening.
Which health services can CHPW members earn rewards for completing? Who is eligible?
Rewards are only available to current CHPW Members. They must meet the age requirements by screening type and be a CHPW member with the eligible plan at the time of the screening.
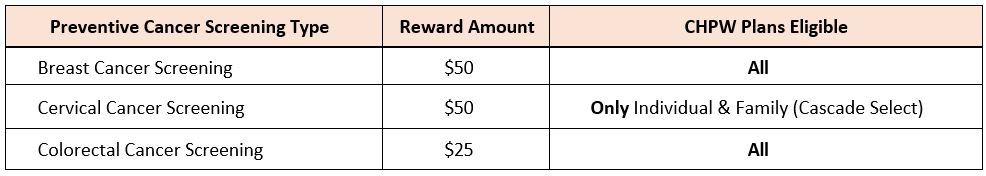
All CHPW health plans offer rewards for certain preventive screenings with MemberFirst™ rewards.

For CHPW Apple Health members, ChildrenFirst™ Rewards for prenatal, postpartum, and well-child checkups are also offered. For help with a member eligibility issue, email [email protected].
What is the reward for each screening and where can gift cards be used?
Reward amounts vary by screening type. Members choose a digital or physical card from Amazon, Albertsons/Safeway, Target.
How often can members earn MemberFirst™ rewards?
Once per year, per screening type, per eligible member. CHPW encourages members to talk to their doctor or health care provider about what type of screenings they should get and how often they should get them.
For Apple Health members, there is a $200 yearly limit for total rewards a member can earn.
Is there a cost for the screenings?
Most preventive screenings are covered by CHPW at no additional cost to members. CHPW follows the regulatory bodies (HCA, Affordable Care Act (ACA), CMS) for preventive services and cost shares.
Visit healthcare.gov, cms.gov, and hca.wa.gov for details.
CHPW Provider Resources and Member Benefit Grids
How do members claim rewards?
It’s all online. Claim rewards within 180 days (about 6 months) of screening or test to qualify by filling out a “rewards submission form”.
In the form, members provide their member number, and information about the completed screening.
Where can members get more information and access the form to claim rewards?
Get answers to common questions and access the reward submission forms for CHPW members:
If you still have questions, call Customer Service for help. Our representatives are available at 1-866-907-1906 (TTY Relay: 711) Monday through Friday from 8 a.m. to 5 p.m.